LUMBAR PLEXUS
I find this block to be one of the few, whether single injection or continuous, where the impact of ultrasound utilization is not as dramatic an improvement as it is with most other nerve blocks. This comes from a few different variables. One, it is usually a deep block, so visualization of structures is on a more gross level of differentiation. Second, it is not as ‘eloquent’ of a block as so many others; we are not placing local exactly between this and that layer or under that structure or between these two nerve roots. With the lumbar plexus block, we are filling a muscle belly with local, so exact guidance of the needle and precise catheter positioning is not as imperative (though clearly, we could choose an inferior needle tip or catheter position). As well, the multiple targets are not immediately adjacent; I know I will likely not be directly ‘on target’ for each nerve root. This is one reason why (among a few) I am not a fan at all of the Axillary Nerve block, especially for catheter placement. Third, I almost hate to admit it, but landmark techniques for this block, I have found, are very good. Most of the time, when I do an out of plane approach with ultrasound, I find that my landmarks would’ve been right on track; it might take me a little longer, but I am on track. After what I’ve written in a lot of other sections on this site, I guess I can’t keep that one.
The other thing that always lurks in the back of my mind is the question of how much more benefit a patient gets with a Lumbar Plexus block (LPB) nerve block compared to other techniques (like Fascia Iliaca) ) given [nonmember]…
REGISTER for FREE to become a SUBSCRIBER or LOGIN HERE to see the full article!
[/nonmember]
[wlm_ismember]
the ‘deep block’ status of a LPB with regards to anticoagulation issues. Consider the use of this block for Total Hip Arthroplasty. I can get the same coverage (Femoral, Lateral Femoral Cutaneous, Obturator) with a Fascia Iliaca block, and I am not at all concerned about the impact (or likelihood) of multiple needle passes. I have done a Fascia Iliaca nerve block multiple times as a ‘Rescue Block’ (See Tip of the Week Section for more on this) for patients that pre-operatively declined a LPB and had great results. I have, at this point, switched totally to doing Fascia Iliaca nerve blocks over Lumbar Plexus for these reasons. I do the Fascia Iliaca for sure afterward because it is a quick block to perform and so I would not have to reposition the patients after a Total Hip Arthroplasty. Further, with using only a LPB (and not adding a Sacral Plexus or Subgluteal Sciatic block in addition), I know that I am not covering all six nerves to the hip joint anyway. The patient will likely have some discomfort in the PACU that will require opioids. What about a ‘third best’ option of just a Femoral Nerve Block in that case? Though I will get even less coverage (better if it is an anterior surgical approach), the Femoral block is simple and carries nearly zero risk (arguably less than a LPB ans similar to a Fascia Iliaca block, anyway). Is it worth it to more reliable cover the Lateral Femoral Cutaneous and Obturator with a LPB? Honestly, if you bolus enough local into a Femoral nerve block, you will probably have a Fascia Iliaca block.What about LPB versus a Femoral nerve block for a Total Knee Arthroplasty?
OK, I’m not saying to avoid this nerve block (either single or continuous) or even to do it without ultrasound. I rarely perform this block anymore, but I do use ultrasound all the time when I do. I’m saying that it is complex to decide when it is appropriate (if at all) given your patient population, your surgeon’s views, your case mix and the current level of expertise within your group. For example, if your surgeon typically uses an anterior approach to Total Hip Arthroplasty, it is much easier to position a catheter for a Lumbar Plexus Block than for a Fascia Iliaca Block. It also makes the positioning for a Parasacral Nerve Block convenient while you are at it, in fact.
It is a block that should be considered (by ASRA guidelines) like an epidural instead of as a nerve block. Like the Tip of the Week comments from January 23, 2012, THE answer does not exist to this question. In fact, there are several ways to scan then perform the LPB block with ultrasound (in vs. out of plane & transverse vs. longitudinal view). Though I may have seemed to have painted a negative picture of the use of ultrasound for this nerve block, I will go on shortly to mention some reasons that I think it is still helpful to use and how it may improve safety.
It is a good practice, especially when learning any new nerve block -and particularly when it is a nerve block that involves significantly altering your ‘non-ultrasound’ technique, to first visualize in three dimensions what is beneath the skin. This should point you toward a ‘common sense’ needle trajectory before you start for you reference. Keep this expectation in your mind when things do not go smoothly, you are starting to make multiple needle passes or you do not see what you think you should see. At these moments, immediately go back to your ‘common sense’ expectation, to make sure you have not gotten off course. With the Lumbar Plexus Block, I still draw my landmarks ahead of time, then I prepare for an ultrasound technique.
With my landmarks identified, I start with a longitudinal paramedian scan of the spinous processes to confirm that I am between L4 and L5, then I turn to a transverse view and look for the transition between the Erector Spinae (and just laterally, the Quadratus Lumborum ) Muscle and Psoas Muscle by rocking and sliding the probe slightly in a cranial and caudal direction. It helps to visualize the transverse process as these muscles are adjacent just below this depth. At times, I am correct in visualizing the nerve roots, but other times, I am fooled by the white reflection from a tendon. Primarily, though, I identify the posterior third of the psoas muscle and aim for that. You can get an idea of this by doing a deeper scan to see the bowels just anterior to the psoas muscle then dividing it in thirds. I move my probe laterally a few centimeters and enter with the needle at a more shallow angle to improve visualization. Because the curvilinear probe detects things laterally, I can still start right next to the probe. If you recognize the depth of your target and move laterally the same number of centimeters, you can advance at a 45 degree angle to reach your target reliably as well. I have also kept the same transverse probe orientation and gone out of plane for larger patients to keep from going through so much tissue in images that were less than desirable. I then use the depth of the transverse process (off screen) to guide my expectant needle depth. I also utilize a longitudinal ultrasound image (not shown here) and direct my needle out of plane between the teeth of the ‘trident sign’ (three transverse processes with adjacent bone shadows below) into the psoas muscle.
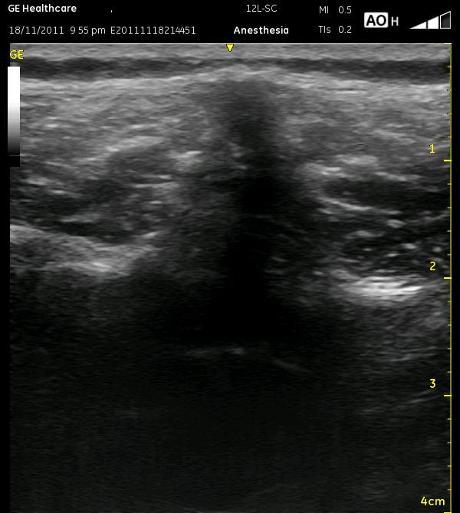
The following ultrasound picture shows a potential misunderstanding which can lead to confusion while scanning and with needle placement. Can you identify the shadow of the Spinous Process, Erector Spinous Muscles and the Transverse Processes? Have a look before you look further at the next ultrasound picture.
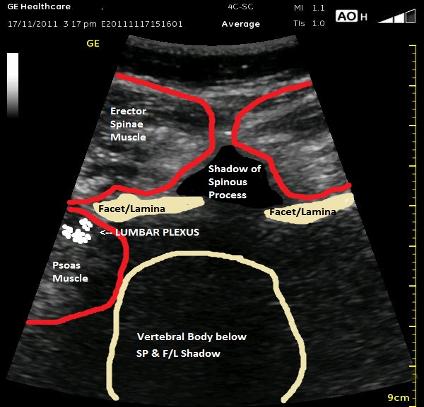
OK, it was a trick question. The white lines immediately lateral to the Spinous Process shadow are actually the Lamina (or maybe Facets). I hope you recognized the other two structures though. This is an easy early misconception in learning this block because we are so focused on locating the Transverse Processes, and we see bones sticking out lateral to the spinous process and think we’re there. The Transverse Processes extend laterally from the anterior aspect of the lamina above the pedicle. The transverse processes are out more lateral and deep to the lamina.

I have mentioned in other sections about the ‘transition stages’ along the way as you are working to rely on ultrasound instead of (or in addition to) nerve stimulation. I want to point out a mistake that can be made here with the LPB. Many people use ultrasound to scan first to get appropriate depths, to determine the distance from midline and to see that they are not over the transverse process. Next they put the probe down to do a standard nerve stimulation approach. This sounds like a simple point, but it can trip you up. Remember that if you scan to determine the depth of the psoas muscle, that number of centimeters is only accurate if you then press your hands into the skin at the same depth that you compressed it with the probe (and often people don’t press the tissue is at all). Normally, one tries to hit the transverse process then walk off and advances the needle a few more centimeters looking for a twitch. If you are lining up the needle over an area where there is no transverse process, then using a predetermined depth for the needle, you never get the confirmatory depth the transverse process would have given you. You may then underestimate the depth of the psoas muscle, and you will make multiple shallow passes, wasting time, hurting your patient and macerating muscle tissue. The other end of this problem is using relatively little probe pressure, then pressing the tissue more with your fingers at the skin. If you miss the lumbar plexus on your initial pass, you may then plunge into something that you really didn’t want to discover. Be sure to watch the video link below for a perspective on how little ‘wiggle room’ there really is.
The ultrasound picture below is a midline transverse view between the Transverse Processes which will allow an out of plane or in plane (medial or lateral) needle approach. For any of these approach, it would be helpful to slide the probe laterally a few centimeters. Notice that the Lumbar Plexus estimation is in the posterior 1/3 of the Psoas Muscle belly. The Spinous Process does reach superficially because the beam is not crossing at its highest point. The Vertebral Body is likely larger than what is represented in the cartoon image, and the medial border of the Psoas Muscle is also estimated due to the bone shadow from the Lamina/Facet above.

I will accept up to 1.0 mA quadriceps twitch; that is, I don’t waste excessive time or try many more passes to try to get it much lower. Encountering a twitch much less than 0.5mA (as well as a lateral to medial needle approach) can be associated with epidural spread of local especially with the relatively high infusion pressures from a bolus. With this block, I am very particular about taking extra time to inject and with very low pressures. Consider this point, however, as it relates to an initial epidural spread. It is very unlikely that the pressure generated by an infusion of 10ml/hr or less will result in an ongoing epidural spread of local. Closely follow patients that have bilateral symptoms of numbness or weakness, confirming that they do not progress (or have symptoms due to an excessive sympathectomy) and that their symptoms resolve. If you are assured that your catheter placement is adequate (and all other things being equal), you may be able to utilize the catheter post-operatively AND there may be an upside in immediate analgesia for that patient.
I’ll leave it with one more technical point on catheter removal. I have been called to the floor a few times by nurses for LPB catheters that wouldn’t come out. I do not excessively thread catheters and do not currently utilize those with metal springs at their distal end, so my worst fears are not real considerations. Although having the patient bend in various directions and injecting sterile saline might have helped to some degree, what I have found is that the ‘hang up’ is almost always very superficial. Gently pulling the catheter taught, then pressing the skin away from the catheter has always worked. Of course, NEVER use excessive force to remove any catheter especially if local anesthetic has been flowing through it recently.
Currently, I do a lumbar plexus catheter for direct approach total hip arthroplasty with a single injection parasacral nerve block. For ‘traditional’ hip arthroplasty (with a single injection parasacral nerve block), distal femur fracture or hip fracture, I do a fascia iliaca catheter, I do a fascia iliaca catheter for some of the reasons mentioned above.
Follow the link below to an ultrasound video demonstrating a transverse Lumbar Plexus scan demonstrating how rocking the probe identifies the appropriate plane in which to direct the needle. It is in greater depth than necessary for the block in order to show the adjacent structures.
[/wlm_ismember]

